This post may contain affiliate links and ads in which we may earn a small percentage of purchases.
Table of Contents
Diverticular disease, a common gastrointestinal condition, particularly in the Western world, encompasses a spectrum of symptoms and potential complications. Understanding the nuances of this disease is crucial for individuals seeking to manage its manifestations effectively.

Anpol42 WikiMedia1. What is Diverticular Disorder?
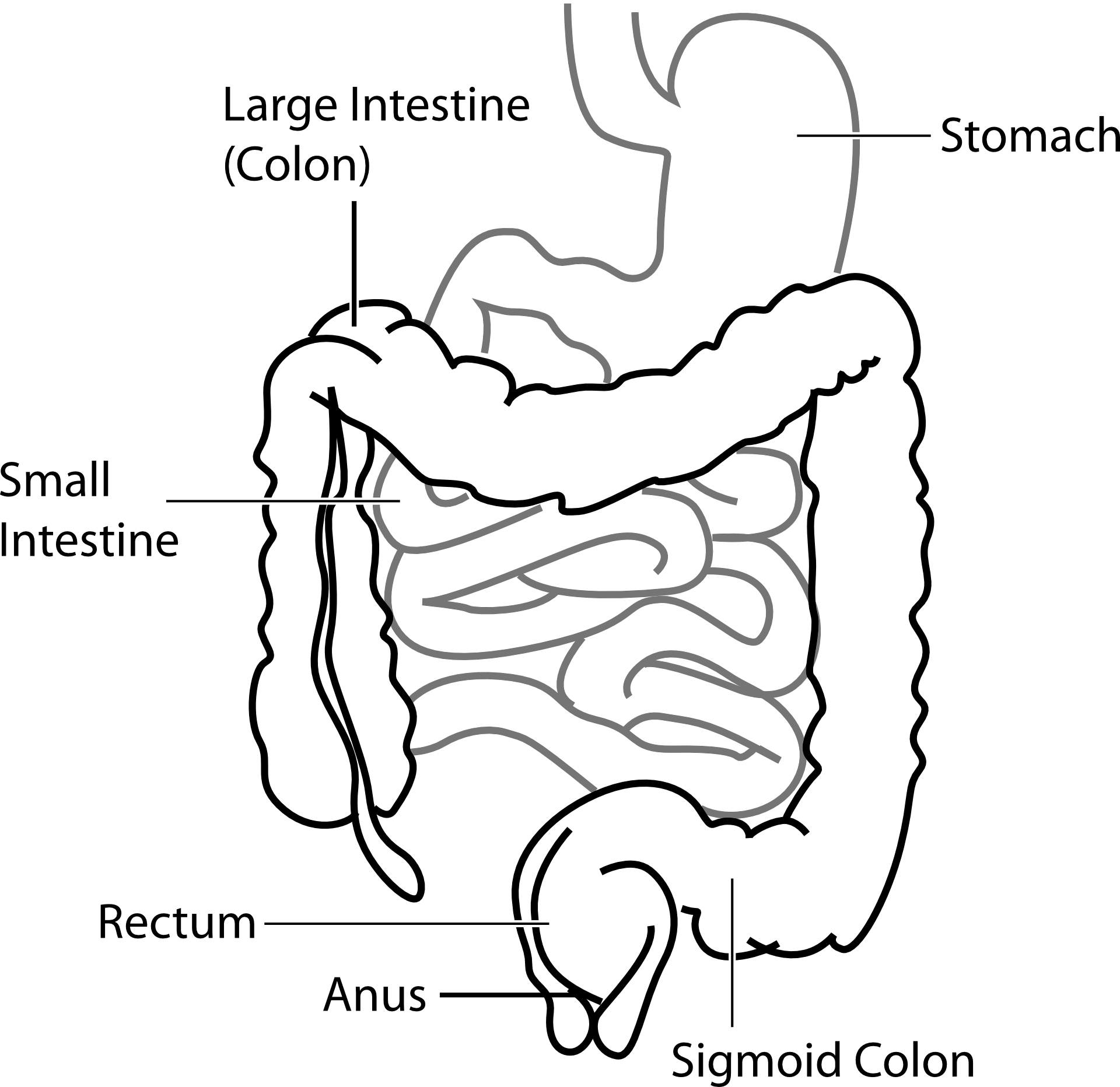
Diverticular disorder refers to the presence of diverticula, small, bulging pouches that can form in the lining of the digestive system, particularly in the lower part of the colon. These pouches are relatively common, especially after the age of 40, and they often don’t cause discomfort or symptoms. However, when complications arise, it’s referred to as diverticular disease (Rezapour, Ali, & Stollman, 2018).
2. The Difference Between Diverticulosis and Diverticulitis
Diverticulosis: This term refers to the mere presence of diverticula within the colon. On the other hand, if these pouches become inflamed or infected, it leads to a condition known as diverticulitis. This inflammation can result in severe abdominal pain, fever, nausea, and a marked change in bowel habits. The complications of diverticulitis can be serious, including abscesses, perforation, and intestinal blockages (Boynton & Floch, 2013).
3. Current Treatments
- Antibiotics to treat infection.
- Pain relievers.
- Bowel rest, where the patient may be advised to stick to a liquid diet for a certain period, allowing the bowel to heal.
- In severe cases, surgery may be necessary, especially if complications like perforations, abscess, or fistula occur.
Treatment for diverticular disease varies based on its severity and symptoms. For diverticulosis, dietary changes, including increasing fiber intake, are often recommended. Diverticulitis, however, might require antibiotics, pain relievers, and sometimes even surgery, especially in severe cases or if complications arise. Recent studies have explored the roles of therapies like mesalamine, rifaximin, and probiotics in managing diverticular disease symptoms (Rezapour, Ali, & Stollman, 2018).
A stainless-steel acupuncture pen and gua sha set.
 View Product
View Product
4. When to Seek Medical Attention
It’s crucial to consult with a healthcare professional if you experience symptoms such as persistent abdominal pain, fever, and an inability to pass stools, as these could indicate complications like infection or even a perforation. Immediate medical care ensures proper management and can prevent further complications.
5. Research on Diverticular Disorder
The prognosis for diverticular disease is generally good with appropriate management. However, the condition can recur. Lifestyle modifications, including diet changes and regular physical activity, are beneficial. Complications, while rare, can be serious and potentially life-threatening, emphasizing the importance of prompt treatment and regular medical follow-up (Boynton & Floch, 2013).
Etiology and Environmental Factors:
- The influence of diet and environmental factors on the onset and progression of diverticular disease is a significant focus. Recent studies have shifted the understanding of diverticular disease from being primarily associated with older Western populations to a more global perspective, recognizing its increasing prevalence across various age groups worldwide.
- Dietary habits, specifically the type and amount of fiber intake, play a crucial role in the disease’s manifestation. Recent analyses indicate that higher dietary fiber consumption, particularly whole fruits and certain types of cereal fibers, is associated with a lower incidence of diverticular disease. Conversely, diets high in red meat, particularly unprocessed red meat, have been linked to a higher risk.
- Other environmental factors, such as smoking, have been found to complicate the outcomes in patients with diverticular disease, leading to a higher incidence of complications.
Management and Treatment:
- The management of diverticular disease is evolving, with a growing emphasis on non-operative and outpatient strategies for uncomplicated cases. This approach includes the use of specific pharmacologic agents aimed at preventing the recurrence of diverticulitis, thereby reducing the need for surgical interventions.
- There is a debate regarding the surgical treatment of diverticulitis, with recent trends questioning the traditional approaches. The focus is on identifying subsets of patients who may not require surgery and understanding the long-term outcomes of conservative management strategies.
Epidemiological Shifts and Genetic Links:
There is an acknowledgment of the changing epidemiology of diverticular disease, with a broader age range affected and a reevaluation of its pathophysiology. Researchers are also uncovering genetic mutations and variations associated with the development of diverticulitis, suggesting a potential hereditary component or predisposition in some individuals.
Diverticular disease is a manageable condition with a generally favorable prognosis, especially when diagnosed early. Ongoing research continues to enhance our understanding and management of this condition, offering hope for even more effective treatments in the future.
The information provided in this article is intended for general knowledge and educational purposes only and should not be considered a substitute for professional medical advice, diagnosis, or treatment.
References:
- Rezapour, M., Ali, S., & Stollman, N. (2018). Diverticular Disease: An Update on Pathogenesis and Management. Gut and Liver, 12(2), 125–132. Retrieved Oct. 17th, 2023 from Link
- Boynton, W., & Floch, M. (2013). New strategies for the management of diverticular disease: insights for the clinician. Therapeutic Advances in Gastroenterology, 6(3), 205–213. Retrieved Oct. 17th, 2023 from Link
- Koprowski, M. A., Affleck, A., & Tsikitis, V. L. (2022). Emerging evidence and recent controversies in diverticulitis: a 5-year review. Annals of Gastroenterology, 35(1), 8–16. Retrieved Oct. 17th, 2023 from https://doi.org/10.20524/aog.2021.0677
- (2022). Diverticular Disease—An Updated Management Review. Gastroenterology Insights, 13(4).Retrieved Oct. 17th, 2023 from https://www.mdpi.com/2036-7422/13/4/33
Medical Disclaimer: This article is for informational and educational purposes only and is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a qualified healthcare provider with any questions about a medical condition or treatment.